AddressBokeljska 7, Belgrade
Contact phone+381 11 3910 112, +381 11 3910 115
Working hoursMonday - Friday, 10AM to 6PM

Sinonimi: Naevus, Nevus
Most moles are harmless skin lesions, but there are moles that have a greater chance of developing melanoma in them, and exactly because of that, regular skin monitoring is a step of great importance in early melanoma detection, as well as detection of other skin cancers.

Moles are presented by an uneven gathering and growth of melanocytic cells in the skin. Melanocytic cells produce the pigment melanin, which gives the skin it’s color and is a natural source of skin protection against damage caused by the Sun’s UV rays. These cells should be evenly distributed throughout our skin (never two of them together), covering the whole surface in an even fashion, with the exception of palms and soles.
A certain number of moles is present as soon as birth, and those moles are called congenital moles, all other moles are considered acquired. The most of them appear during the first 20 years of life, other moles can form later in life.
In time, most of the moles will go slightly lighter in color and become elevated. Moles can go darker in some periods, i.e. after sun tanning, in teenagers and during pregnancy. Certain moles will develop hairs. A small number of moles may spontaneously disappear over time. Some of them will not change during life.
Typical moles (common or regular) are usually up to 6mm in diameter, one color ranging from light brown to black, symmetrical, with clear borders. They develop during the first 20 years of life, their size corresponds to our body growth, but they don’t significantly change their appearance and color.



Typical mole can be flush to the skin, elevated (above the skin) or hanging, it can be with or without hairs.



It can be soft or hard to the touch.
It’s typical no matter if it’s there since birth, if it developed in early youth or later during life. The fundamental characteristic of it’s typicality is that it doesn’t change!
Synonyms: Dysplastic nevus
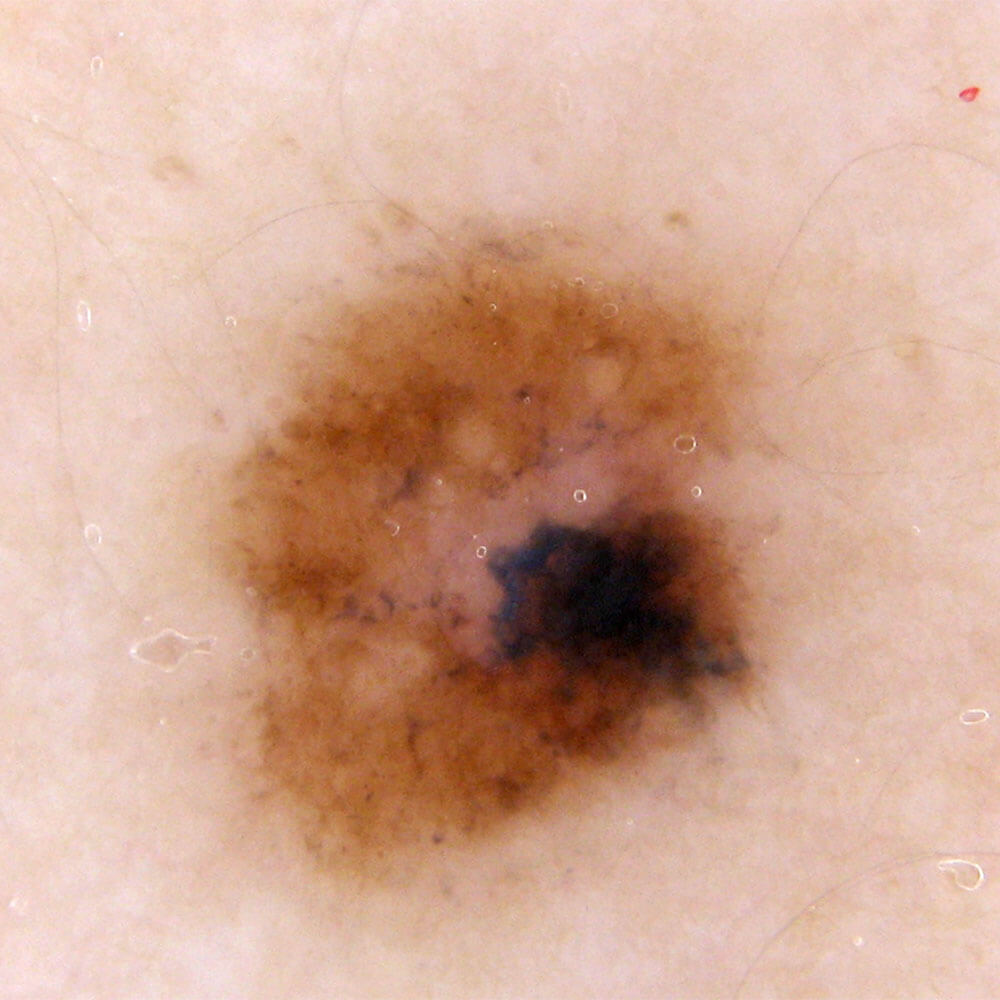
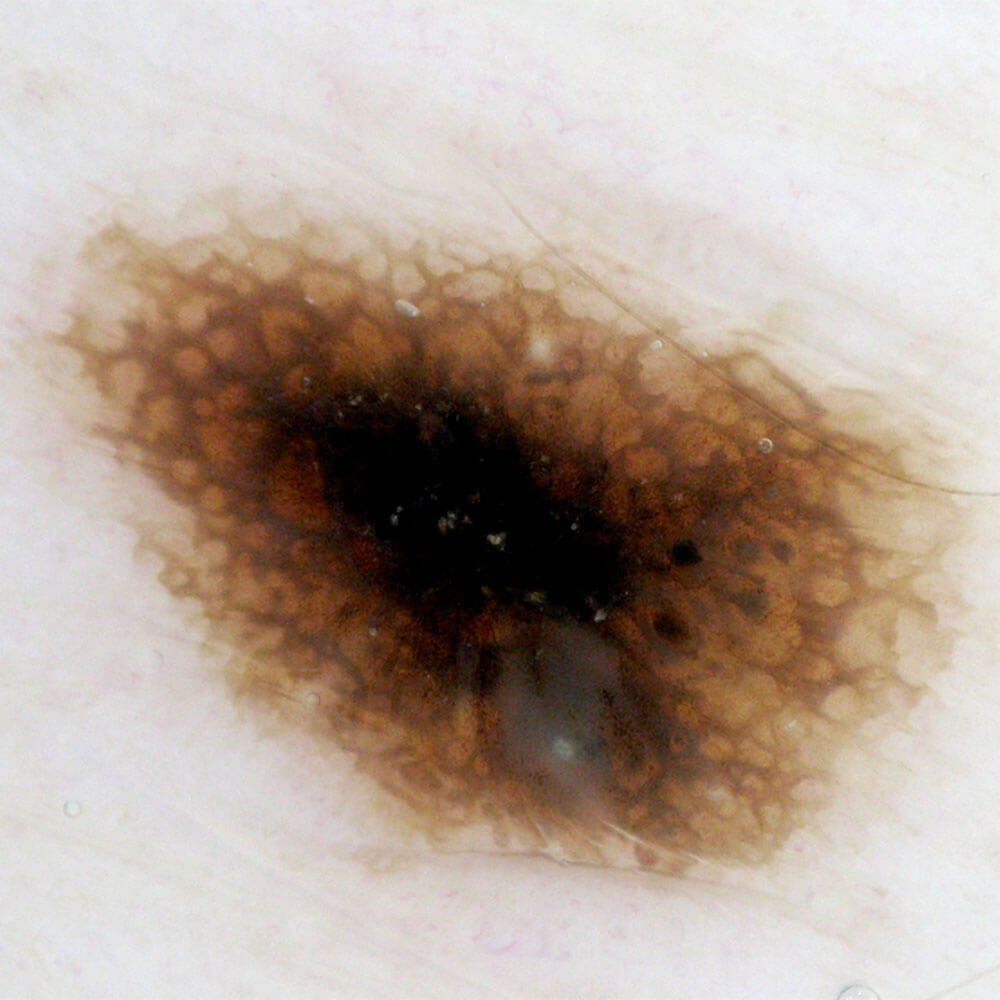
Atypical mole differs from other moles by it’s size, color and shape.
Atypical mole is larger than 6mm in diameter, it has multiple colors (at least 2 colors), it’s irregular in shape (asymmetrical) and the borders are discontinued, jagged or unclear. These are the features that can be seen by naked eye.
Histopathological characteristics, that a doctor-pathologist can see in atypical moles are completely different and bring this mole very close to melanoma, such mole is known as a Dysplastic mole (Dysplastic nevus is it’s histopathological diagnosis).


Due to these characteristics, many consider it a “precancer”, essentially a state that directly leads to melanoma. However, the fact stands that atypical moles present only a greater possibility for developing melanoma, but not each of them will become one. Out of all melanomas, half are developed in existing atypical moles, and the other half of all melanomas are developed in completely healthy skin.
Sysnonyms: Atypical mole syndrome
All people who have more than 100 moles of which at least one is a histopathologically confirmed atypical mole (dysplastic nevus) have AMS. These persons have a greatear risk for developing melanomas but it doesn’t necessarily mean that all of them will develop melanomas during life.


Synonyms: congenital melanocytic nevi (CMN)

These are moles that are present at birth or in the first days after birth. Size – wise, they can be classified as small (up to 1.5cm in diameter), medium (from 1.5 to 10cm), large (from 11 to 20cm) and gigantic (larger than 20cm in diameter) (table 1).
Statistics say that small congenital nevus occurs in 1 out of a 100 newborns a that gigantic nevi occur in 1 out of every 500 000 newborn children. In relation to he sex, they are somewhat more common in girls than in boys. (1.3-1).
The probability of a melanoma forming in a congenital nevus grows with it’s size, therefore all large and gigantic nevi are advised to be removed preventively.
| small | < 1.5cm | |
| medium | 1.5-10cm | |
| large | 11-20cm | |
| gigantic | G1 | 21-30cm |
| G2 | 31-40cm | |
| G3 | > 40cm | |
The examination of moles based on their looks as well as on the base of their features is called a clinical examination (by eye or by loupe). The doctor doesn’t make a diagnosis on the basis of a clinical examination, he rather divides them into typical (low risk) and atypical ( high risk for development of melanoma). After a clinical examination the doctor decides on which moles are atypical and potentially suspicious and suggests dermoscopic diagnostics be appplied to those moles.
Clinical examination is advised to everyone, but before others, to people with risk factors for development of melanoma and/or with suspicious moles.
ABCDE rules of clinical examination entail visual (by eye) noticing of the following appearance characteristics and features of the mole:
In order for You to assess whether Your mole is assymetrical by Yourself, compare the shape and colors (top half with bottom half, inner half with the outer one). In a symmetrical mole those halves are very similar, and are notably different in asymmetrical ones.
Of course, not every asymmetrical mole is suspicious of melanoma.

Asymmetrical mole

Symmetrical mole
Moles usually have a well defined border.
Mole with a discontinued border is the one that doesn’t have a clear junction in relation to the surrounding skin or it’s discontinued, jagged.

Discontinued border

Preserved border
Moles are usually single colored. If a mole has at least 2, and especially if it has 3 or more colors, it most certainly needs to be subjected to a detailed dermoscopic analysis.

Mole with at least 2 colors

single color mole
Detailed dermoscopic analysis is neccesary on all moles larger than 6mm in diameter.

Mole diameter under 6mm

Mole diameter over 6mm
If You notice that Your mole is suddenly growing, changing shape or color, leaking, crusting, if it gets inflamed, itches, hurts or gets injured, it is neccesary to report it to Your doctor as soon as possible, and he will examin You and direct You towards a dermoscopy if it’s needed.

Grows and changes shape

Crusts

Bleeds
Dermoscopy is the latest, most modern, noninvasive, painless method for early diagnostics of melanoma and all other pigmented skin lesions. This method provides, through superficial contact microscopy, better «in vivo» visualisation of structures in the epidermis and dermis, which are of significance for making a diagnosis. This method found it’s application in the diagnostics of melanoma. In comparison to previous, clinical diagnostics, dermoscopy improves the accuracy of making a diagnosis of melanoma by 20 to 30%, which provides the accuracy of dermoscopy in the range from 92 to 99%, confirmed by histopathology.
Except for diagnosing melanoma, dermoscopy is used in diagnostics of all skin lesions, such as: mole, basal cell carcinoma, seborrheic keratosis, dermatofibroma and angioma.

Most common techniques for removing moles are:
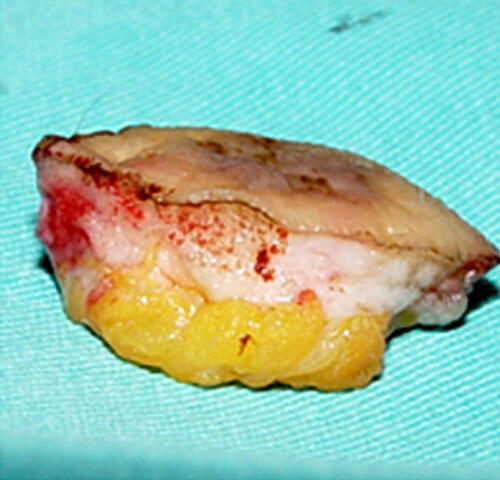
Excision is a basic surgical technique for removing all skin lesions. This technique removes the entire lesion with a part of the healthy surrounding skin and subcutaneous fatty tissue.
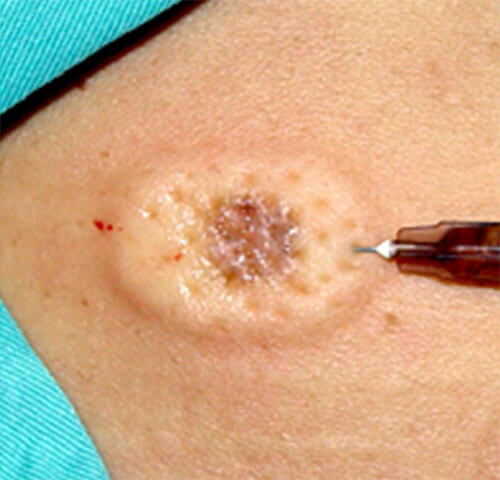
local anesthesia

skin incision

ekscidirana promena u “zdravo” po širini
ekscidirana promena u “zdravo” po dubini

defect after excision

primarna sutura: direktno zatvaranje rane
This is a technique that involves removing the mole with radio waves and / or a scalpel, leaving a minimal scar on the skin.
Whenever this technique can be applied, we choose it, because it aesthetically gives excellent results.

Before

After
Other techniques of removing skin lesions are:
Moles are commonly removed by an excision (cutting them out). Layered excision (shave) is used only for esthetic removal and only in specialized facilities which meet the required diagnostic, surgical and histopathological conditions. Other techniques are used in cases of extremely large moles, when the remaining defect after removal is too big to be directly closed (sutured end to end).
Skin and mole monitoring encompasses the measures of early diagnostics, tracking and follow-up of moles, and these are: selfexamination of moles, dermoscopic monitoring and mapping of moles on the body.
Selfexamination or selfcontrol of moles is an important element in the prevention of developing melanoma. The basis of selfexamination is spotting atypical and risky moles, by examining moles head to toe. In order to be able to independently control and track Your moles, some education is required, as well as cooperation with Your physician. Selfexamination is very usefull, especially on persons who have at least one of the risk factors for developing melanoma. Selfexamination is sufficent to be done monthly. Yearly follow-ups with a doctor are advised to any person that practices selfexams.
Dermoscopic monitoring is the most important element of good mole tracking. Only through the method of digital dermoscopy is it possible to effectively and precisely track all moles on Your skin, with clear microscopic magnification of the structures inside. It essentially entails repeat dermoscopies of moles at regular follow up visits, and clear notice of any developing changes in them, with seeing similarities and differences in the tracked lesion.
Mapping of moles and all lesions of the skin by regions on the body in the form of digital photographs is called “body mapping”. During this procedure it’s necessary to acquire quality digital images of all the skin regions where all lesions can be clearly seen, no matter what their size is. When there is a body map present, You get the option of detailed tracking of moles over a lifetime.
Skin and mole monitoring enables discovery of initial changes in existing moles as well as discovery of completely new atypical pigmented skin lesions, and thus enables applying early diagnostics and prevention of developing melanoma.
Laser, for the time being, should not be used for removing moles, because after laser removal , moles can’t be sent for histopathological analysis.
Every mole needs to be sent for histopathological analysis after removal so we can know whether it’s a benign, atypical or malignant lesion.
When the HP analysis tells us that the removed mole was a dysplastic nevus, we have directly prevented the formation of melanoma, but we have created a task to regularly and precisely track the patient in the future.
And in case of melanoma diagnosis, of great importance is an extensive histopathological finding that determines the further course of the treatment.
Yes, removing moles is completely safe. Removing moles can’t cause the cancer (melanoma).
That, above all depends on the type of the mole on one side, and patient’s risk factors on the other side. In short terms, some moles are suitable for removal, others can be tracked for some time, and then decided on whether they should be removed.
Yes, removing moles for esthetic reasons is completely safe if we have honored the standards for treating moles, being the following three conditions: firstly, we have done Diagnostics on the mole, secondly, used adequate removal technique ,thirdly, sent the removed mole for histopathological analysis
Yes, a biopsy of a mole is completely safe and is used rarely, only in cases of unclear dermoscopic diagnosis.
No, removing moles under local anesthesia is completely safe. Moles are commonly removed under local anesthesia, and other types of anesthesia are used only in rare cases, like when removing a gigantic congenital nevus.
Best way of protecting moles is the same way as You protect the rest of Your skin from excessive UV radiation.
In short: If You never get red from exposing to the Sun, if You gradually get a bronze tan,If You never go as far as getting a maximum tan for Your complexion, if You don’t have any signs of skin Sun damage – You have protected Your mole and the rest of your skin adequately.
No, You shouldn’t cover Your moles up with anything, they should be treated as the rest of the skin.
Because melanoma, one of the most dangerous carcinomas, can look like a mole, especially at an early stage, and on the other hand, because melanoma can develop in a preexisting mole in about 50% of the cases.
Injured mole should firstly be protected from further injury and possible infection. Therefore, it’s best to wash it with lukewarm, previously boiled water and cover it up with a sterile gause or bandage. It would be best to contact Your physician for a check up, and if possible report to the nearest specialized facility that deals wtih moles and provides services such as digital dermoscopy.
Educating Yourself on selfexamination following the ABCDE clinical rules will provide You with a tool to spot any changes on a mole, thus early discovering any risky moles. All moles that are undergoing sudden changes are considered suspicious moles. Sudden changes of a mole are called Evolution, and this envelops the following: sudden growth, change of size or shape, change of color, leaking, bleeding or crusting, inflammation, itching, pain or injury. Occurence of any of these signs presents a risk, and the more the signs the higher the risk of developing melanoma on a mole is.
Congenital moles are not protected from the possibility of developing melanoma in them just by birth. So, as with any other mole, congenital mole carries the same potential risk for developing melanoma, and the risk grows with the size of the congenital mole.
This misconception most probably derives from the fact that in our culture we look on moles as a natural feature, even a feature that brings good fortune, and not as lesion on the skin that’s essentially an “error” we have no need for.
There is nothing safer than removing a mole. By removing a mole, there is no way the character of the mole could be changed, meaning, there is no way for a mole to convert to a melanoma just by removing it. This is the most common misconception, and unfortunately it is present not only in general population, but in a part of medical personnel.
The origin of this misconception is probably related to the well established opinion that injuring a mole is a trigger for the development of melanoma or that injuring during life has caused a new, dangerous mole to form.
Elevated moles are not any more dangerous than moles that are level with the skin. The moles that used to be level with the skin and started to suddenly elevate (grow in height) are dangerous, those who have Evolution.
Elevated moles are more exposed to daily trauma, hence they present a basis for potential fear that the malignant transformation process in to a melanoma will be triggered by injury.
Existence of hair in a mole is not a characteristic on which a “safety” of a mole can be judged on. Safe moles are the ones that do not have any of the risk features by ABCDE rules of clinical examination.
In short terms, moles that are single colored, symmetrical, smaller than 6 mm in diameter and do not change are considered safe.
The origin of this misconception is probably derived from the fact that that earlier, melanomas were only diagnosed at late stages, when all the skin structures in them, even hairs, have perished. The fact is that now, when we are able to detect a significant percentage of melanomas at an early stage, we find melanomas with hairs in them as well.
This is the most common fear, but also a misconception.
There is no clear evidence that there was a change in the benign character of a mole after injuring it, meaning, the injury was the reason for developing a melanoma.
The first sign of developing melanoma in a mole is in the form of sudden superficial or vertical growth, change of color or noticing some of the other characteristics from the ABCDE rules of clinical examination.